

It is a life-threatening situation associated with rapid deterioration of left ventricular function, often leading to cardiogenic shock, and ultimately, death. Although multiple cases of simultaneous coronary occlusion have been reported and various mechanisms have been postulated, the exact mechanism remains unclear. AMI due to simultaneous total occlusion of multiple coronary arteries, including the left main coronary artery, is rare. STEMI caused by the simultaneous thrombosis of multiple coronary arteries is rare and difficult to identify using 12-lead electrocardiography (ECG). ST-elevation myocardial infarction (STEMI) is usually caused by acute thrombosis of only one epicardial artery, which is termed the culprit vessel. A combination of judicious medical treatment, efficient primary percutaneous coronary intervention, and early mechanical support device insertion is crucial to improve the survival rate of patients with this disease.Ĭoronary plaque rupture and acute thrombosis are the primary mechanisms of acute myocardial infarction (AMI).

ConclusionsĪcute double-vessel coronary thrombosis, a serious event with a high mortality rate, requires prompt diagnosis and management to prevent complications such as cardiogenic shock and ventricular arrhythmias.
Fifty-seven days after admission, he had New York Heart Association class II heart failure and was transferred to a rehabilitation hospital. An Impella CP was inserted during the procedure. The patient successfully underwent primary percutaneous coronary intervention with ballooning and stenting for both arteries. Emergency coronary angiography revealed total occlusion of the proximal left anterior descending artery and right coronary artery. Electrocardiography revealed ST-segment elevation in leads II, III, aVF, and V1–V6. We report the case of a 58-year-old man who presented with vomiting and chest pain complicated by cardiogenic shock and complete atrioventricular block. Therefore, immediate revascularization and adequate mechanical circulatory support are required. It is difficult to identify using 12-lead electrocardiography and usually leads to cardiogenic shock and fatal outcomes, including sudden cardiac death. The GUSTO-III study showed no significant difference in 30-day mortality for the agents (7.47% vs 7.24%, p=0.61), respectively.Simultaneous thrombosis in more than one coronary artery is an uncommon angiographic finding in patients with acute ST-segment elevation myocardial infarction. Based on the open-artery hypothesis and previous data showing an absolute difference of 15% in 90-minute TIMI grade 3 flow between the agents, it was anticipated that mortality would be lower with rPA than with accelerated tPA.
Timi iii flow trial#
The recently completed GUSTO-III trial compared accelerated tPA with reteplase (rPA).
Timi iii flow plus#
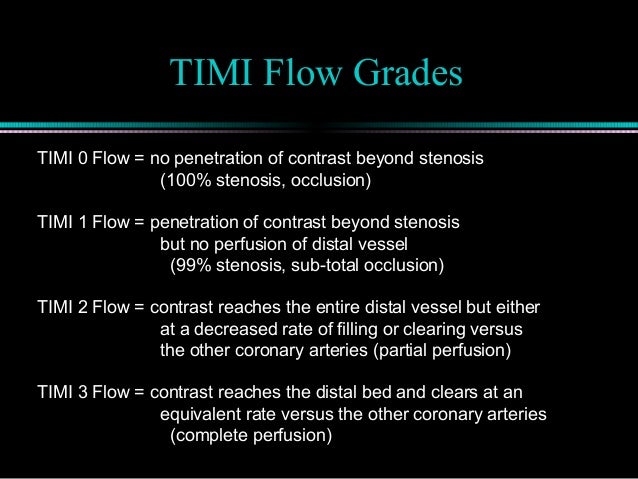
However, despite significantly higher 90-minute TIMI grade 3 flow (54% vs 32%) with accelerated tPA versus SK plus intravenous heparin, the absolute difference in mortality rate was less than 1%. The angiographic substudy of GUSTO-I provided strong evidence for the relationship between 90-minute thrombolysis in myocardial infarction (TIMI) grade 3 flow and lower mortality.
Timi iii flow Activator#
This theory was tested in the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries (GUSTO-I) study. This discrepancy, in part, led to the open-artery hypothesis that early and sustained infarct-related artery patency improves outcome. However, only recently did clinical trials compare tissue plasminogen activator (tPA) and streptokinase (SK), and only one study showed a difference in mortality between them. Many large, placebo-controlled trials conclusively recorded improved survival with thrombolytics in the treatment of acute myocardial infarction. Thrombolytic therapy dates back to animal studies performed in the early 1940s, although clinical trials did not begin until the early 1980s.


 0 kommentar(er)
0 kommentar(er)
